Contents:
Over the past few years, the healthcare sector has been grappling with unprecedented challenges brought on by digital transformation, the pandemic, shifting demographics, and rising patient expectations. For healthcare executives, staying competitive means making strategic investments in the right technologies to enhance patient care while managing operational costs and compliance with ever-evolving regulations. Meanwhile, product managers in health tech companies face continuous pressure to keep up with rapid innovation, identify technology gaps, and align development strategies with market demands.
In this rapidly changing landscape, it’s essential to recognize promising innovations and evaluate which solutions offer immediate, tangible advantages for your business.
With combined expertise in augmented reality technology and healthcare app development, Andrew Makarov, an AR expert and solution architect, and Andrii Sulymka, who has over a decade of experience in developing web and mobile applications with a focus on health and wellness domains, will explore the latest healthcare software innovations and offers strategic advice on making informed technology investments.
Trend #1: Modernizing Legacy Healthcare Systems to Drive Innovation and Meet Market Demand
Healthcare providers increasingly recognize the need to modernize legacy systems to stay competitive, meet regulatory demands, and foster innovation. Outdated IT infrastructure hampers scalability, increases operational costs, and introduces significant cybersecurity risks. In a 2024, report by Bain & Company and KLAS Research, three-quarters of U.S. healthcare providers and payers reported increasing IT spending over the past year. The report surveyed 150 organizations and predicts this trend will continue, driven by a heightened focus on technology post-pandemic.
Financial impact of modernization
Modernizing legacy systems offers substantial long-term ROI despite the initial costs:
- Reduce IT maintenance costs by up to 40%, as reported by Forrester in a 2024 study.
- Achieve 20-30% improvement in operational efficiency, translating into cost savings in staff time, resource management, and patient throughput.
- Mitigate cybersecurity risks, thereby reducing the financial impact of potential breaches. The Ponemon Institute notes that the average cost of a healthcare data breach in 2023 was $9.23 million, making modernization essential to avoid these expenses.
Forrester’s 2024 study indicates a 175% ROI within 3-5 years for organizations prioritizing modernization. For example, St. Mary’s Health System significantly upgraded its EHR from a monolithic to a microservices-based architecture. This migration to microservices resulted in a 30% increase in clinical efficiency and reduced system downtime by 25%, directly contributing to improved patient care outcomes and a $2 million reduction in annual IT costs. This case underscores the financial viability of modernization initiatives, demonstrating that upfront investments can yield substantial returns over time.
Similarly, Kaiser Permanente, one of the largest healthcare organizations in the U.S., embarked on a $4 billion IT modernization initiative. By integrating cloud solutions with AI-powered predictive analytics, Kaiser Permanente improved patient flow across its network of hospitals and reduced operational costs by $1.5 billion annually. This example illustrates how large-scale modernization efforts can enhance operational efficiency, unlock new revenue streams, and reduce redundancies.
Challenges in Implementation
The path to modernization is not without obstacles:
- Cost of Transition: The initial cost of modernizing legacy systems can be significant, particularly for small and mid-sized healthcare organizations. Migrating data from old systems and implementing new platforms may involve downtimes and temporary service disruptions.
- Staff Training and Adoption: Legacy systems are often deeply embedded in daily operations, and shifting to new systems requires extensive staff training. Resistance to change is common, and organizations may struggle with user adoption without proper change management strategies.
- Data Migration and Integration: Transferring large volumes of data from outdated systems to new platforms can be complex. Data migration requires rigorous testing to ensure data integrity, and failure to do so can lead to data loss or inconsistencies.
- Compliance and Security Risks: Ensuring new systems comply with healthcare regulations like HIPAA and GDPR can be challenging, especially when dealing with cloud-based solutions. Careful attention must be given to data encryption, access controls, and audit trails to ensure compliance during and after migration.
Long-Term Projections: As cloud-based systems, AI, and IoT become more integrated in healthcare, organizations that delay modernization may struggle to maintain operational efficiency. A Gartner report forecasts that healthcare providers who fail to modernize their systems by 2026, will see a 20% increase in cybersecurity incidents and a 15% reduction in patient satisfaction due to outdated service delivery methods.
Practical Advice on Implementing Modernization
- Start with High-Impact Areas: Start by assessing which components of your legacy systems can be upgraded or replaced. MobiDev’s Healthcare Software Modernization Guide can advise you on the process, ensuring a seamless transition while minimizing disruptions.
- Engage in phased modernization: Break down the process into manageable phases, starting with the most critical systems like EHRs and patient management tools.
- Leverage Cloud Solutions: Migration to cloud-based platforms enhances scalability and security, providing a robust foundation for future innovation.
- Collaborate with experienced partners: Working with experienced providers ensures seamless integration of legacy systems with modern technologies. MobiDev’s Software Modernization Services help healthcare organizations transition smoothly, with minimal disruption to operations and a focus on compliance and data security.
Trend #2: IoT and Wearables Gain Traction in Healthcare
The Internet of Medical Things (IoMT) is at the forefront of personalized healthcare. IoMT allows continuous, real-time monitoring of patient health metrics through wearables, biosensors, and remote diagnostic tools. According to Grand View Research, the IoMT market is expected to grow at a 20.4% CAGR through 2030, enabling better disease management, predictive healthcare, and proactive interventions. The growth is primarily driven by the increasing adoption of connected devices like wearable external medical devices, implanted medical devices, and stationary medical devices, along with advancements in remote patient monitoring and telemedicine solutions. The demand for these technologies has surged due to the need for continuous patient monitoring and the growing integration of 5G and AI technologies in healthcare infrastructure.
Wearables in Healthcare
Wearable devices also use AI in mental health monitoring. Smartwatches, fitness trackers, and biosensors transform healthcare by enabling continuous patient monitoring. A 2024 Gartner study found that 3 out of 10 working-age individuals now use a wearable device, offering healthcare providers real-time patient data such as heart rate, blood oxygen levels, and glucose levels.
For instance, platforms like Mindstrong analyze data from users’ smartphones or wearables, such as typing speed, voice patterns, and sleep patterns, to detect early signs of mental health issues like depression or anxiety. This allows for continuous, real-time monitoring and intervention, providing more timely support to individuals in need.
Financial Impact of IoT in Hospitals
IoT is not only improving patient care, it is also optimizing hospital operations. Philips IntelliVue Guardian Solution, for instance, uses IoT-enabled wearables to monitor patient vitals, reducing mortality rates by 18% and significantly cutting the time needed for emergency interventions. Hospitals using IoT for asset tracking and inventory management have reported a 30% reduction in equipment loss, saving millions in operational costs annually.
Practical Advice on Implementing IoT
- Start with high-impact use cases: Focus on IoT applications with immediate benefits, such as remote patient monitoring or asset management.
- Data security: IoT devices often operate on open networks, making them vulnerable to cyberattacks. Secure these devices with encryption, firewalls, and access control measures.
- Address accuracy challenges: Ensure IoT devices are properly calibrated and regularly updated to maintain data accuracy.
For a complete end-to-end IoT solution, MobiDev’s IoT Development Services help healthcare organizations build secure, scalable IoT systems.
Trend #3: AI Continues to Revolutionize Healthcare
Artificial intelligence in healthcare has become a cornerstone innovation, and its potential continues to expand. According to a 2024 report by MarketsandMarkets, the global AI in healthcare market is expected to reach $45.2 billion by 2026, up from $10.4 billion in 2021. The report notes that AI adoption is accelerating due to its potential to enhance diagnostic accuracy, streamline clinical workflows, and personalize patient care.
AI in Data Management
One of AI’s most impactful applications is in AI data management. AI algorithms can analyze EHR data to identify patterns and trends, helping healthcare providers streamline workflows, improve documentation accuracy, and enhance clinical decision-making. For example, Epic EHR, one of the leading Electronic Health Record systems, has integrated AI through Microsoft’s Azure OpenAI service, enabling natural language processing (NLP) capabilities that assist in clinical note generation, patient summaries, and predictive analytics. Epic has also been expanding its AI initiatives, focusing on predictive models that forecast patient outcomes such as readmission risks or potential complications.
Another EHR provider, Veradigm (formerly Allscripts), has embraced AI by utilizing Azure OpenAI’s GPT-4 to enhance clinical workflows, personalize patient care, and improve population health management. This AI integration allows physicians to create personalized treatment plans more efficiently, engage patients through tailored recommendations, and improve overall treatment effectiveness.
Additionally, Cerner (now part of Oracle Health), a major competitor in the EHR space, has integrated Oracle’s AI and machine learning technologies into its platforms. These AI-driven solutions help healthcare providers predict patient outcomes, optimize hospital operations, and provide more proactive care management through real-time clinical insights.
AI in Diagnostics and Drug Discovery
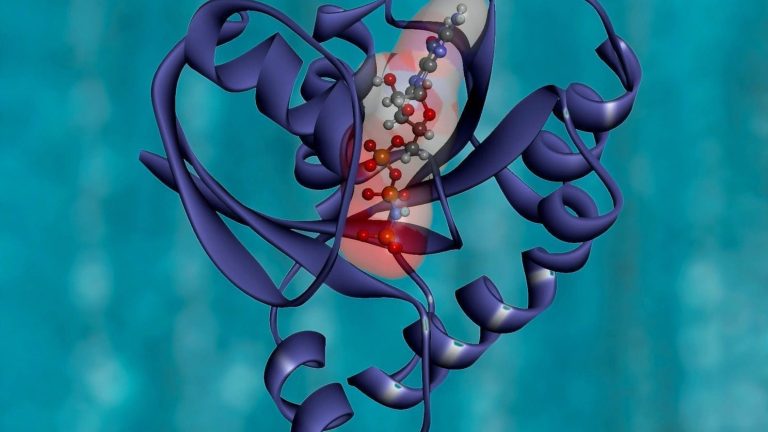
AI transforms drug development and diagnostics by improving information processing and decision-making efficiency. AlphaFold2, developed by DeepMind, has made a breakthrough in predicting 3D protein structures with unprecedented accuracy. Available via Google Colab, it uses machine learning and multi-sequence alignments to predict protein folding. With over 200 million structures predicted to date, it provides a crucial resource for drug discovery.
Similarly, DeepAffinity, a semi-supervised model combining recurrent and convolutional neural networks (RNNs and CNNs), forecasts drug-target binding affinities. It uses labeled and unlabeled data to encode molecular and protein sequences, outperforming traditional models like random forests and ensembles.
AI continues to be viewed as a promising solution, with its limitations and benefits, in cancer diagnosis. Our engineer conducted complex research on utilizing AI for cancer detection by processing whole slide images or WSI. Working with WSI appears challenging due to the giant resolution of the image. While WSI scans are extremely informative, it takes hours of scrupulous zooming in and out, scrolling from area to area, to conduct the examination. AI can process WSI using computer vision and convolutional neural networks. This approach supports healthcare professionals by spotlighting the area of interest where potential cancer cells can be located, reducing the time for diagnostics.
However, the implementation of AI for the WSI examination not only brings solid outcomes but also requires specific preparation for model training. This aspect should be thoroughly considered during the adoption of AI across the healthcare industry since WSI scanners have become a conventional part of medical institutions.
Practical Advice on Implementing AI in Healthcare
Implementing AI in healthcare requires a structured and strategic approach to ensure its success and compliance with industry regulations. Here are the key steps to consider when integrating AI technologies in healthcare operations:
- Data Quality and Preparation: Any successful AI model’s foundation lies in the quality and comprehensiveness of its training data. Healthcare data is complex and often comes from various sources such as EHRs, medical imaging, genomics, and wearable devices. To ensure your AI system delivers accurate results, your development team should work closely with experienced data scientists who can clean, preprocess, and structure this data. Additionally, ensure that you have high-quality, representative data that covers a wide range of scenarios, reducing bias and improving generalizability.
- Collaboration Between Experts: AI implementation should be an interdisciplinary effort involving healthcare professionals, data scientists, AI engineers, and IT experts. While the AI system will handle complex predictions and diagnostics, it must work harmoniously with healthcare providers who understand the clinical context. At MobiDev, we emphasize collaboration between domain experts and AI engineers to tailor solutions that meet the unique needs of healthcare organizations.
- Ethical AI Development: The usage of AI in healthcare raises significant ethical considerations, particularly concerning patient data privacy. To safeguard patient information, healthcare organizations must adhere to stringent regulations such as HIPAA in the U.S. and GDPR in the EU. At MobiDev, we focus on developing AI systems with robust security measures—from encryption protocols to role-based access control—to ensure that sensitive health information is always protected.
- Explainable AI (XAI): AI algorithms often function as “black boxes,” making it difficult for healthcare providers to understand the reasoning behind their outputs. However, transparency is significantly critical in a healthcare context when decisions impact patient outcomes. Implementing explainable AI (XAI) models allows healthcare professionals to interpret AI-driven decisions, providing clarity and fostering trust between patients and providers.
- Integration and Scalability: Implementing AI is not a one-off task. AI systems should be designed to integrate seamlessly with existing healthcare infrastructure, such as electronic health records (EHRs) and telemedicine platforms. Additionally, scalability is essential for organizations planning to expand their AI capabilities across multiple departments or locations. MobiDev’s AI Consulting services are designed to ensure smooth integration and scalability, helping healthcare organizations evolve with changing technological landscapes.
Planning to create an AI healthcare product?
Align your business goals with tech capabilities and market demand
AI Healthcare Consulting ServicesTrend #4: Telemedicine Continues to Drive the Evolution of Remote Care
The telemedicine revolution, spurred by the COVID-19 pandemic, has proven to be more than a temporary shift. As healthcare delivery continues to evolve, telemedicine is positioned to become an integral part of the care continuum. According to a 2024 report by Fortune Business Insights, the global telemedicine market is expected to reach $185.6 billion by 2026, driven by demand for remote care and advancements in telehealth infrastructure.
The Growing Role of Telemedicine
Telemedicine has expanded beyond primary care, encompassing mental health, dermatology, and pediatric specialties. Remote monitoring tools, virtual consultations, and telemedicine apps have become essential for delivering care to patients in underserved or rural areas. Additionally, telemedicine reduces the strain on healthcare systems by minimizing in-person visits and lowering operational costs.
When combined with healthcare kiosks that facilitate essential health screenings without needing a doctor’s visit, telemedicine can greatly alleviate the workload on hospital staff and create more space for seriously ill patients.
Mobile Health (mHealth)
Another significant development in telemedicine is the rise of mHealth (mobile health) applications. These apps enable patients to take charge of their health by providing real-time data and insights. For instance, apps like Stepler reward users for physical activity, encouraging them to adopt healthier lifestyles. Applications in the mHealth space are improving patient engagement and generating valuable health data that can be integrated into EHRs.
Practical Advice on Implementing Telemedicine:
Developing a telemedicine application for your healthcare organization requires thoughtful planning around compliance, technology choices, and data security. Here’s how you can navigate the process:
-
Complying with Regulations
One of the most significant challenges in telemedicine, is adhering to regulations like HIPAA in the U.S. and GDPR in the EU. During the pandemic, some restrictions were temporarily eased. Still, healthcare providers must ensure that their telehealth platforms comply with all regulatory requirements, especially concerning storing and transmitting protected health information (PHI). For example, you need to use HIPAA-compliant hosting solutions. If you’re developing your telehealth app or using third-party services like Zoom for video conferencing, you must verify that the platform meets industry data security and encryption standards, and more.
For further guidance on how to ensure compliance, check out MobiDev’s guide on HIPAA-Compliant Software Development, which offers a comprehensive checklist to guide your implementation.
-
Using WebRTC for Secure Video Conferencing
For telemedicine apps that require custom video conferencing features, WebRTC (an open-source API) is a robust solution that facilitates real-time communication while maintaining data privacy and security. It is ideal for creating a dedicated telemedicine app, ensuring secure audio, video, and data transmission.
-
Cloud Hosting and Data Storage
While many cloud storage services offer reasonable levels of security, not all are suitable for handling protected health information. Adopting HIPAA-compliant cloud solutions that support EHR integration and data encryption is essential to ensure your telemedicine platform’s functionality and security. MobiDev provides custom cloud hosting solutions that meet stringent healthcare industry standards, enabling seamless integration with EHRs and other patient management systems.
-
Key Functionalities to Consider
Beyond teleconferencing and secure data hosting, consider adding features that enhance both patient engagement and operational efficiency, such as:
- Appointment scheduling
- Secure messaging
- Location services
- Integration with wearables (e.g., Google Fit, Apple HealthKit)
- Healthcare provider reviews and visit history management
Integrating these features enhances patient experience and adds value to your telemedicine platform.
Trend #5: Extended Reality (XR) in Healthcare Settings
Extended reality – an umbrella term that includes augmented, virtual, and mixed reality, can be innovative and beneficial in the healthcare industry. From assisting surgery to improving telehealth applications, AR and VR technologies can improve the healthcare industry substantially. These immersive technologies are used for applications ranging from surgical training and rehabilitation, to remote consultations and medical education.
According to a 2024 GlobalData report, the global healthcare XR market is expected to reach $9.5 billion by 2028, growing at a CAGR of 23.6% from 2024 to 2028. This growth is driven by increasing demand for personalized healthcare solutions and the need for more efficient medical training.
AR and MR in Healthcare
Augmented reality (AR) and mixed reality (MR) revolutionize various healthcare scenarios. In medical education, AR-based simulations allow students to practice complex procedures in risk-free virtual environments. For example, HoloAnatomy, developed by Case Western Reserve University, uses MR to teach anatomy, providing a fully interactive 3D model of the human body.
AR in surgical assistance is also becoming more widespread. A notable example is AccuVein, which uses AR to make vein visualization easier, leading to more efficient and accurate blood draws. Surgeons increasingly use AR headsets to overlay critical information directly into their field of vision during operations, improving precision and reducing the risk of errors.
VR in Medical Training and Therapy
Virtual reality (VR) has become invaluable for both medical training and therapeutic applications. Platforms like Osso VR provide immersive surgical simulations, helping surgeons practice procedures in a risk-free virtual environment. A study published by Harvard Medical School in 2024 found that surgeons trained using VR saw a 230% improvement in procedural performance compared to traditional methods.
In rehabilitation, VR is gaining traction to enhance patient engagement. For instance, InMotion’s Corpus VR platform combines motion-enabled games with physical therapy exercises to create a more interactive patient experience. These systems improve adherence to rehabilitation programs and collect real-time data to personalize treatment plans. Additionally, VR therapy has emerged as a powerful tool for treating mental health disorders like PTSD and anxiety. The Virtual Reality Medical Center uses immersive environments to help patients confront and manage their fears in a controlled, virtual setting.
Practical Advice on Implementing XR in Healthcare
Implementing AR/VR technologies in healthcare requires collaboration with experienced developers who understand the unique needs of the healthcare industry. From ensuring HIPAA compliance to designing user-friendly interfaces, XR applications need to meet both medical and regulatory standards.
Here are some key steps for successful XR implementation:
- Pilot Programs: Start with small-scale pilot projects to test the effectiveness of XR in your organization. This allows for fine-tuning based on real-world feedback before scaling up.
- Integration with Existing Systems: Ensure that XR applications integrate seamlessly with existing healthcare systems.
- Collaborate with Experts: Partnering with experienced developers is essential for creating tailored XR solutions that address the specific needs of healthcare professionals and patients. MobiDev’s AR Consulting Services can help you design and implement custom XR solutions that improve patient care, enhance medical training, and integrate seamlessly into your healthcare infrastructure.
Trend #6: Data Security as a Priority for Healthcare Providers
According to IBM’s 2024 Cost of a Data Breach Report, the average cost of a healthcare data breach rose to $10.93 million, the highest across all industries for the fourth consecutive year. Between 2023 and 2024, over 700 organizations worldwide experienced significant data breaches, with healthcare accounting for 25% of all incidents.
One notable example is the Truepill data breach in 2023, which impacted over 2.3 million individuals. Truepill, a provider of mail-order prescriptions for pharmacies, faced repercussions not just in financial penalties but also in eroding consumer trust. Such incidents underscore the importance of compliance with regulations like HIPAA and GDPR, as well as the need for robust healthcare security measures.
Ensuring Compliance with HIPAA and GDPR
Healthcare providers must ensure that their systems are HIPAA-compliant to avoid hefty fines and data breaches. This includes maintaining end-to-end encryption, multi-factor authentication, and role-based access controls for sensitive data. For organizations serving patients in the EU, GDPR compliance is critical. The GDPR mandates strict data protection measures, with severe penalties for non-compliance.
Examples of Advanced Security Solutions in Healthcare
Facial Recognition for Access Control: One of the most secure ways to ensure authorized access to healthcare systems is through biometric solutions like facial recognition. These technologies are increasingly used in hospitals and clinics to securely authenticate medical personnel accessing sensitive patient records and devices. For example, Cedars-Sinai Medical Center implemented facial recognition technology in 2024 to streamline access to patient data, reducing unauthorized access incidents by 30%.
End-to-End Encryption for ePHI: With the rise in telemedicine, healthcare providers must ensure that electronic Protected Health Information (ePHI) is protected during remote consultations. WebRTC is a popular technology that offers encrypted video conferencing solutions, ensuring patient data remains secure during virtual visits. Integrating WebRTC with a HIPAA-compliant platform can significantly enhance data protection.
Challenges in Implementation
Although adopting robust security measures is essential, healthcare providers face several challenges in implementing these solutions:
- Integration with Legacy Systems: Many healthcare providers still rely on legacy IT systems, which may not support the latest security technologies. Upgrading these systems can be costly and time-consuming but is crucial for maintaining security standards.
- Complex Vendor Management: When healthcare providers work with third-party vendors for telemedicine or cloud services, ensuring that these vendors meet security and compliance requirements is critical. Obtaining vendor business associate agreements (BAAs) is necessary but can be intricate and cumbersome.
- User Experience vs. Security: Balancing ease of access for healthcare professionals and the robust security measures needed to protect patient data can be challenging. For example, adding multiple layers of security, such as multi-factor authentication, can slow down the workflow and lead to frustration among medical staff. Finding the right balance is essential.
Practical Advice on Implementing Data Security in Healthcare
- Implement Layered Security: Use a multi-layered security approach that includes encryption, access controls, and regular audits to ensure compliance. Ensure all telehealth platforms are HIPAA-compliant and secure.
- Leverage Biometric Authentication: Incorporating biometric solutions like facial recognition for accessing sensitive data can add an extra layer of security without sacrificing user experience.
- Work with Experienced Partners: Partnering with developers specializing in healthcare security ensures your systems are compliant and robust.
Trend #7: AI in Mental Health Applications
As we mentioned before, AI is making significant strides in healthcare, and particularly in mental health for early diagnosis and personalized treatment. AI is proving to be a valuable tool in detecting neurodegenerative diseases like dementia at an early stage. Conditions like Alzheimer’s disease, which can impair communication, reasoning, and memory, often develop over decades without noticeable symptoms. Early diagnosis, however, is crucial for mitigating the progression of these diseases and improving patient outcomes.
Thanks to advances in deep learning and AI-powered audio processing, it’s now possible to analyze human speech for early signs of dementia. AI models can be trained to distinguish between the speech patterns of healthy individuals and those exhibiting signs of cognitive decline. These tools hold promise for early screening and self-assessment of Alzheimer’s, potentially identifying the disease years before severe symptoms appear.
According to a 2024 study by researchers at Boston University, AI models analyzing speech patterns were able to detect early symptoms of Alzheimer’s disease with an accuracy rate of 78.5%, years before traditional diagnostic methods would have identified the condition. This early detection allows for timely interventions and could potentially slow the progression of the disease.
AI-Powered Mental Health Solutions
Breathhh, an AI-driven Chrome extension, provides personalized mental health exercises tailored to an individual’s online behaviors and web activity. By continuously monitoring and analyzing user interactions, Breathhh identifies the ideal moments to suggest stress-relieving practices, seamlessly integrating self-care into daily routines. This innovative approach merges AI technology with practical mental health support, simplifying the process of mental wellness management.
Another example is Woebot Health, which uses AI to provide real-time emotional support through conversation-based therapy. Woebot has shown efficacy in treating symptoms of depression and anxiety, providing users with accessible, on-demand care. Such platforms highlight the potential of AI in making mental health care more proactive and personalized.
Financial Impact and Market Growth
The global market for AI-driven mental health applications is expected to reach $3.3 billion by 2027, growing at a CAGR of 20.6% from 2024 (Global Market Insights Inc). This growth is driven by increasing demand for accessible mental health care, particularly in regions where in-person therapy is not readily available. AI-based platforms reduce the burden on healthcare professionals, offering scalable solutions to a growing mental health crisis.
Practical Advice on Implementing AI in Mental Health:
Implementing AI in mental health care requires careful attention to both technological and ethical considerations. Here are key steps for integrating AI effectively:
- Ensure Patient Privacy and Compliance: Mental health data is sensitive, and AI-powered apps must comply with HIPAA and GDPR. Data encryption, anonymization, and role-based access control are essential for safeguarding user privacy.
- Develop Transparent AI Models: Using explainable AI (XAI) in mental health applications is critical to ensure that users and healthcare professionals understand how AI-driven decisions are made. This increases trust in the platform and improves user engagement.
- Leverage Personalization: AI can offer real-time, personalized recommendations to users based on their behavior and mental state. This enhances the efficacy of the platform and allows for more tailored mental health interventions.
- Collaborate with Experts: Partnering with experienced AI consultants and engineers ensures the technology aligns with clinical needs and regulatory standards. MobiDev’s AI Healthcare Consulting Services help healthcare organizations develop AI-driven mental health solutions prioritizing patient privacy and treatment efficacy.
Future of Healthcare Technology in 2026 and Beyond
Looking ahead, the future of healthcare technology promises groundbreaking innovations such as 3D-printed organs and smart pills that monitor patient health in real time. As these technologies evolve, healthcare organizations must invest in modernizing their systems and adopting emerging technologies to stay ahead of the curve.
With the right technology vendor, healthcare providers can unlock the full potential of these advancements, driving better patient outcomes and improving operational efficiency. For organizations ready to embrace the future, MobiDev offers a range of healthcare app development services to support the implementation of these cutting-edge technologies.